If someone told you that a 20-minute medical test literally could save your life, wouldn’t it be foolish to refuse it? Unfortunately, millions of Americans are doing just that when they fail to get periodic colon cancer screening.
Result: Each year, up to 57,000 Americans die unnecessarily from the disease.
Here’s what you must know to protect yourself against colon cancer
Screening works
Almost all malignancies of the large intestine and rectum start out as premalignant polyps, flat or mushroom-shaped growths that are harmless but may become cancerous. If a polyp is detected and removed, cancer will not develop. That’s why screening regular exams to detect polyps or cancer in its earliest stages is crucial.
The most recent screening guidelines, published by the US Multi society Task Force on Colorectal Cancer in February 2003, recommend screening for all men and women beginning at age 50. If you have already had surgery for polyps or colon cancer or if you have inflammatory bowel disease, such as ulcerative colitis or Crohn’s disease your risk for colon cancer is increased and you should have colonoscopy on a schedule determined by your doctor.
• Colonoscopy every 10 years
This screening test is the most accurate and has been shown to prevent 85% to 90% of colon malignancies.
Many health insurance plans now pay for screening colonoscopy, as does Medicare. Without health insurance, the procedure costs about $3,000.
Unfortunately, colonoscopy has a reputation for being embarrassing and painful. Both criticisms are overblown. Most patients say colonoscopy is not nearly as bad as they had expected. What’
What’s involved:
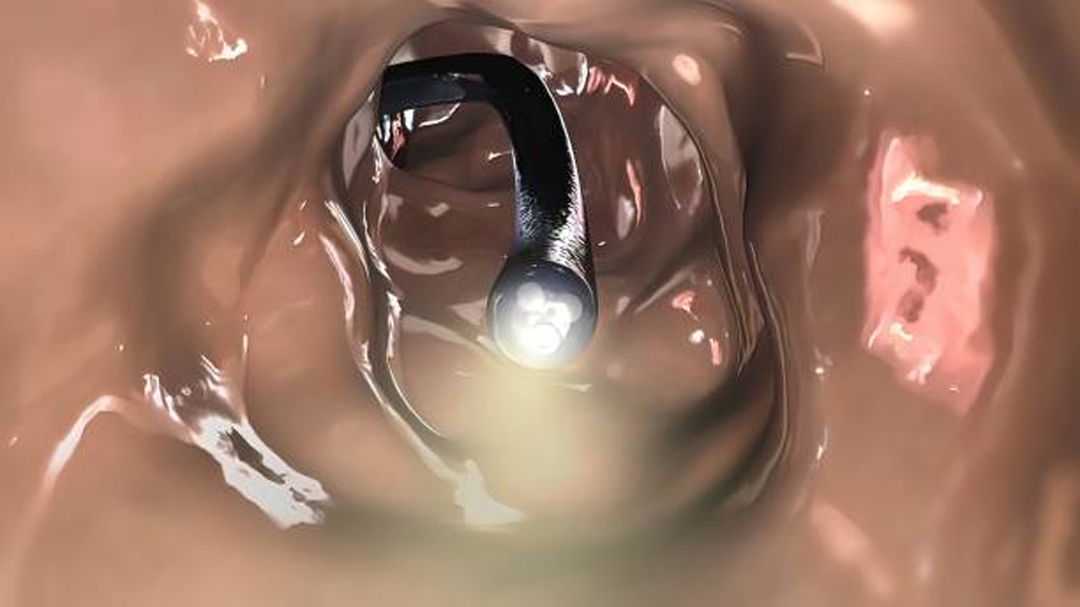
While you are sedated, a flexible, one-half-inch diameter tube that employs digital video optics is threaded through the anus and passed through the large intestine, enabling the doctor to see your entire colon lining on a video monitor. The procedure itself usually takes no more than 20 minutes.
Many people find the preparation, which involves laxatives to empty the bowel, much more unpleasant than the colonoscopy itself.
Until recently, the standard bowel preparation method involved drinking four liters of a bad-tasting colon-cleansing solution, such as golytely, the night before. Newer products now make the process less unpleasant.
• Phospho-soda
It also tastes bad, but you only take several tablespoons dissolved in liquid the night before and the morning of the procedure.
Helpful: While you can mix it with any clear liquid, most patients prefer to mix it in ginger ale to make it more palatable.
• Visicol
It contains the same ingredient but is in tablet form. Instead of downing a liquid solution, you swallow a total of 40 tablets in multiple doses.
Helpful: Whatever bowel prep method you use, consume at least three eight-ounce glasses of fluid the night before to prevent dehydration. You can drink any liquid, but a sports drink that contains electrolytes is preferred.
• Sigmoidoscopy every five years
This test is less invasive than colonoscopy and requires less preparation (an enema the night before and the morning of the procedure) and no sedation. Because the procedure is less thorough than colonoscopy, it identifies only 50% of colon malignancies.
What’s involved:
A flexible tube, like that used in a colonoscopy, is passed through the lowest third of the large intestine (sigmoid colon), where half of all tumors occur.
Sigmoidoscopy appeals to people who don’t want to be sedated. The procedure, which costs about $400, is also less expensive than colonoscopy.
Important: On a subsequent day, you should return to take a barium enema, followed by an X-ray, to view the remaining two-thirds of the colon. A barium X-ray costs about $500.
Although sigmoidoscopy combined with a barium X-ray screens the entire colon, it is still less accurate than colonoscopy.
• Fecal occult blood test once a year
People who don’t want to undergo colonoscopy or sigmoidoscopy can opt for this test. It is the least accurate screening option and only reduces colon cancer rates by one-third. Typical cost: $5
What’s involved:
A chemical applied to stool samples detects traces of blood, which would suggest the presence of polyps or tumors. No preparation is required, but you must avoid certain foods (such as red meats and broccoli) for three days and medications (such as aspirin) for a week before to ensure accuracy. Since the test detects blood, taking aspirin, which can cause internal bleeding, could trigger a false positive.
Some people find the procedure unpleasant because it involves using a small wooden stick to smear small bits of your own stool on specially treated cardboard. If blood is detected, you’ll need to have a colonoscopy.
New test
Virtual colonoscopy uses computed tomography (CT) to provide detailed radiographic pictures of the colon. It is relatively noninvasive, requires no sedation and can be done at your radiologist’s office. It does require the same kind of preparation as colonoscopy. This test is less accurate than conventional colonoscopy—it detects 75% to 80% of polyps larger than one centimeter, but just 40% to 50% of smaller ones. Health insurers will not pay for it. Typical cost: $900.
It may be a good option for people with heart or lung disease, for whom sedation can be risky.







